Navigating the Challenges of Healthcare Economics: Key Issues Facing Providers and Patients. Explore The key challenges in healthcare economics that both providers & patients face. Understand The issues affecting costs & care today!
What is Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients & how does it work?
Navigating healthcare economics requires understanding system dynamics. It involves balancing costs, patient access, & quality care. Providers assess reimbursement models, while patients weigh options for affordability. Important aspects include value-based care, insurance coverage, & policy impacts. These factors shape decisions for both sides in healthcare.
Brief history of Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients
Healthcare economics evolved significantly over decades. Initially, an emphasis lay on fee-for-service models. These early systems often led To high costs with questionable outcomes. Over time, shifts occurred towards value-based care approaches. Policymakers & providers aimed for improved efficiency & patient satisfaction.
How To implement Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients effectively
Implementing effective strategies requires a multi-faceted approach. Providers should analyze current practices & identify inefficiencies. Engaging patients in decision-making enhances outcomes. Data analytics play a crucial role in measuring success. Encouraging collaboration among stakeholders fosters a supportive environment.
Key benefits of using Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients
Benefits include improved patient outcomes & reduced costs. Streamlined processes lead To more efficient care delivery. Increased transparency builds trust between providers & patients. Enhanced resource allocation allows for targeted healthcare interventions. Ultimately, this approach aims for healthier populations.
Challenges with Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients & potential solutions
Many challenges exist in navigating healthcare economics. Rising costs continue To strain budgets for both providers & patients. Complex regulatory environments can create confusion. Solutions involve better education & system transparency. Innovative technology may offer new efficiencies that address these challenges.
Future of Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients
Future trends indicate a shift towards patient-centered care. Increased focus on preventive measures enhances public health outcomes. Advancements in technology will further streamline processes. Collaboration across sectors could drive innovative solutions. Adaptability remains essential as healthcare continues evolving.
Table of Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients
| Key Issues | Impacts | Potential Solutions |
|---|---|---|
| Cost Management | Affordability concerns | Value-based care models |
| Access Issues | Limited provider options | Telehealth solutions |
| Quality of Care | Inconsistent patient experiences | Standardized protocols |
| Regulatory Complexity | Confusion among providers | Clear guidelines & support |

Navigating Challenges in Healthcare Economics
Healthcare economics encompasses various complexities faced by both providers & patients. Many issues require careful consideration as healthcare systems evolve. As a professional in this field, I witnessed firsthand how economic factors impact healthcare delivery & accessibility. This awareness drives ongoing discussions about emerging themes in healthcare economics.
Recent studies reveal crucial insights about healthcare economics. For an in-depth look at key insights, consider exploring this resource available online. Various factors shape costs, access, & quality of care. Providers often grapple with navigating reimbursement models, regulatory constraints, & patient needs.
Understanding Healthcare Costs
Healthcare expenses continue rising, creating significant challenges. Various elements contribute, including administrative costs, pharmaceutical pricing, & technology advancements. Addressing these concerns requires awareness from all stakeholders. Providers must stay informed about market trends & cost management strategies. Patients should also understand their role in controlling expenses through informed decisions.
Price transparency plays a crucial role in addressing cost-related challenges. Greater transparency can empower patients. When individuals know prices upfront, they make better choices regarding their healthcare services. However, achieving transparency remains difficult due To complex pricing structures & various payers involved.
Moreover, a shift from fee-for-service models To value-based care changes economics. Value-based care focuses on patient outcomes, incentivizing providers. This model seeks To improve health while controlling costs. Understanding this shift is essential for patients as well, especially regarding available treatment options & associated expenses.
Influence of Regulations
Regulatory frameworks significantly affect healthcare economics. Policymakers seek To balance access, affordability, & quality. Various laws govern healthcare services, impacting reimbursement rates, providers, & patients alike. Compliance with these regulations poses challenges for many organizations.
For instance, regulations surrounding Medicare & Medicaid dictate reimbursements for care provided. These regulations often impact how services are delivered & which treatments are prioritized. Changes in legislation can create uncertainties for providers & patients alike, making navigation challenging.
Furthermore, regulations surrounding insurance markets influence access & affordability. Mandates for coverage types impact what services are available. Patients must stay informed about their rights under these regulations. Increased awareness encourages active participation in healthcare decision-making.
The Role of Technology
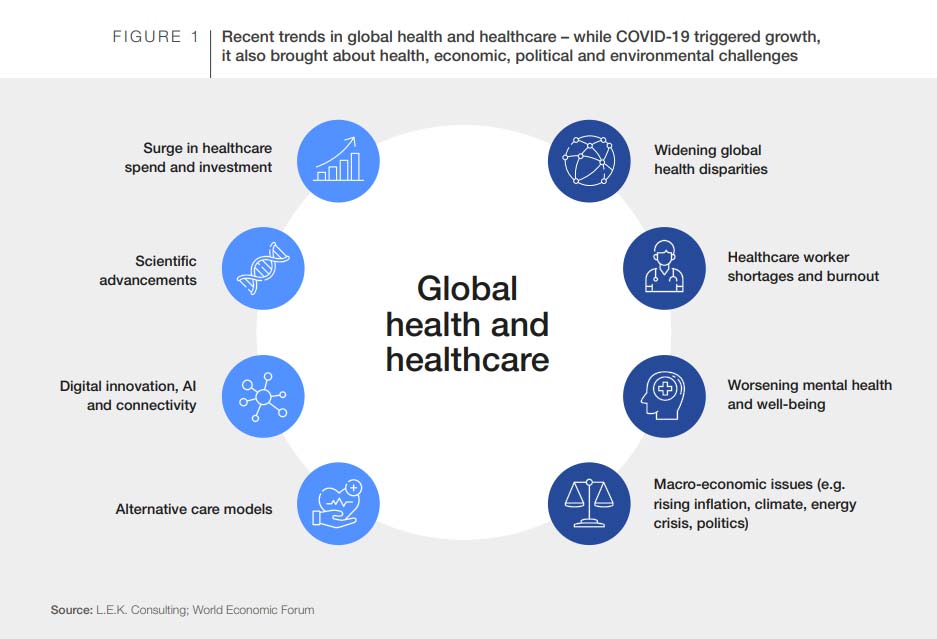
Technological advancements revolutionize healthcare delivery & access. Telemedicine, electronic health records, & AI systems enhance efficiency & patient experience. However, integrating technology into existing systems presents challenges. Providers must adapt To new systems, which require substantial investment & training.
Moreover, patients benefit from enhanced access through technology. Telehealth services reduce barriers for individuals in remote areas. These services increase timely access To specialists & providers. Nevertheless, issues surrounding data privacy & security arise as technology expands. Both providers & patients must remain vigilant.
Additionally, technology influences costs in various ways. While initial investments may be high, efficiency gains can lead To long-term savings. Understanding this balance becomes essential for stakeholders navigating economic challenges. Technology adoption may reduce costs, but organizations must ensure alignment with patient care objectives.
Shifting Consumer Expectations
Consumer expectations in healthcare experience significant changes. Individuals demand more convenience, personalization, & transparency from providers. These evolving expectations affect how services are delivered. Providers must integrate patient-centered approaches into their models, enhancing satisfaction & care quality.
Patients increasingly seek value in their healthcare experiences. Accessing information regarding providers, treatments, & costs has never been easier. This shift necessitates responsiveness from healthcare organizations. Meeting these expectations requires innovative approaches in service delivery & communication.
Moreover, social determinants of health play a critical role in overall patient satisfaction. Factors such as socioeconomic status, education level, & community resources shape health outcomes. Recognizing these influences allows providers To create holistic care models that address patient needs effectively.
Healthcare Workforce Dynamics
The healthcare workforce experiences challenges amidst economic pressures. Provider shortages persist in various specialties, impacting quality & access. Burnout & job dissatisfaction among healthcare professionals further complicate this landscape. Addressing workforce challenges directly affects patient care & providers’ economic sustainability.
Recruitment & retention strategies are essential in combating workforce shortages. Organizations must invest in employee well-being, professional development, & supportive work environments. This investment not only enhances job satisfaction but also improves patient care quality & organizational performance.
Additionally, understanding workforce dynamics becomes vital. An aging population increases demand for services, which strains existing resources. Innovations in team-based care can help alleviate some pressures by enhancing collaboration among healthcare professionals. This collaborative approach can improve outcomes while managing costs effectively.
Impact of Public Health Trends
Public health trends affect healthcare economics significantly. Emerging health issues create demand for services, altering market dynamics. From mental health crises To chronic illnesses, addressing these trends requires adaptation from providers & patients alike. A focus on prevention & wellness becomes paramount.
Furthermore, robust public health initiatives can mitigate economic pressures. Early intervention reduces costs associated with chronic disease management. Organizations must collaborate with public health agencies To ensure effective communication about emerging trends & care strategies. These collaborations foster better outcomes for communities.
Finally, research plays a crucial role in understanding public health impacts. Organizations must continuously evaluate interventions & treatments. Leveraging data analytics enhances decision-making processes & identifies areas for improvement. Organizations adapt their strategies based on emerging evidence, ultimately benefiting both providers & patients.
Strategies for Cost Management
Effective cost management strategies are vital for providers facing economic challenges. Organizations can analyze operational efficiency, supply chain management, & revenue cycle optimization. Addressing inefficiencies often leads To notable cost savings. Understanding spending patterns empowers providers in strategic decisions.
Opportunity for telehealth expansion represents another area for cost management. By optimizing virtual care options, organizations can enhance accessibility & convenience. This innovation can decrease operational costs associated with maintaining physical spaces while improving patient satisfaction.
Collaboration with payers & stakeholders also encourages cost management. Engaging with insurance providers To refine reimbursement models fosters a collaborative atmosphere. Organizations can identify bottlenecks, aligning financial incentives. Streamlining processes enhances efficiency across entire systems, benefiting all involved parties.
Patient-Centric Care Models
Emphasizing patient-centric care models fosters improved economic outcomes. Organizations that prioritize patients’ needs develop stronger relationships & encourage loyalty. Cultivating trust leads patients To seek care from familiar providers. As a result, these providers benefit from consistent patient engagement & lower turnover rates.
This focus supports shared decision-making in treatment plans. Engaging patients in their healthcare encourages active participation, resulting in better adherence To prescribed regimens. Patients who feel empowered are more likely To make informed choices that align with their personal health goals.
Additionally, organizations that adopt patient-centric models often experience positive reputations. Positive word-of-mouth referrals contribute To brand loyalty & attract new patients. Fostering a culture of care focused on individual needs ultimately enhances both financial stability & patient outcomes.
Upcoming Trends in Healthcare Economics
Anticipating future trends allows stakeholders To prepare for shifts in healthcare economics. An emphasis on personalized medicine will likely transform treatment paradigms. As genetic & biomarker tools evolve, tailored treatment options become more prevalent. This shift may lead To improved outcomes & cost-effectiveness in long-term care.
Moreover, advancements in artificial intelligence & data analytics will transform decision-making. These technologies enable providers To analyze trends, predict patient needs, & enhance resource allocation. Adopting these innovations supports proactive approaches in managing healthcare costs & facilitating better outcomes.
Lastly, an increased focus on social determinants of health will shape strategies in healthcare delivery. Addressing these factors holistically will lead To more equitable care. Organizations must actively involve communities in addressing social issues affecting health economics, ensuring sustainable improvements moving forward.
What is health care economics?
Health care economics is a field of study that examines how resources are allocated within The health care sector, including The production, distribution, & consumption of health care services. It focuses on understanding various factors that influence health care costs, access, & quality.
Why is health care economics important?
Health care economics is crucial because it helps policymakers, providers, & patients understand The financial aspects of health care delivery. This understanding can lead To improved policies & practices that enhance The efficiency & effectiveness of health care systems.
What are The main issues in health care economics?
Main issues in health care economics include rising costs, health care access disparities, The impact of health insurance, price variations for medical services, & The economic evaluation of health care interventions & technologies.
How do health insurance models affect health care economics?
Health insurance models significantly impact health care economics by influencing patient access To services, health providers’ reimbursement rates, & overall health care expenditures. The model adopted can dictate The structure of payment systems & The level of financial risk shared between providers & payers.
What is The role of market forces in health care economics?
Market forces play a role in health care economics by affecting supply & demand for services, influencing pricing, & driving competition among providers. However, due To The unique nature of health care, these forces often behave differently compared To traditional markets.
How does The concept of elasticity apply To health care economics?
Elasticity in health care economics refers To how sensitive consumers are To changes in prices or income. For instance, demand for health care services may be inelastic, meaning that changes in price do not significantly alter The quantity demanded due To The necessity of care.
What are The implications of health care spending on The economy?
Health care spending has substantial implications on The economy, affecting government budgets, influencing employment in health-related sectors, & impacting household finances. High spending may lead To trade-offs in other areas of public spending & economic growth.
What is cost-effectiveness analysis in health care economics?
Cost-effectiveness analysis is a method used To evaluate The costs & health outcomes of different medical interventions. It informs decision-makers about which health care strategies provide The best value for money based on The health benefits delivered relative To The costs incurred.
How do social determinants influence health care economics?
Social determinants, such as income, education, & social support, significantly influence health care economics by shaping health status, access To care, & overall health care costs. Addressing these determinants is essential for reducing health disparities & improving health outcomes.
What are The effects of digital health technologies on health care economics?
Digital health technologies can enhance health care economics by improving efficiency, reducing costs, & increasing access To care. These technologies can streamline operations & support better patient-provider communication, ultimately leading To improved health outcomes.

Navigating The Challenges of Healthcare Economics: Key Issues Facing Providers & Patients
Understanding Healthcare Economics
Healthcare economics involves various factors. Providers & patients encounter unique challenges. Rising costs burden both parties. Governments regulate healthcare markets, aiming for equitable access. Providers face financial pressures while delivering care. Patients often struggle with high expenses. Economic theories apply here, impacting policy decisions. Understanding this landscape requires awareness of current trends.
Multiple stakeholders influence healthcare economics. Payers, providers, & patients each play vital roles. Insurance companies control reimbursement rates. This dynamic affects provider revenue streams. Additionally, technological advancements shape costs significantly. Innovations provide efficiency, yet often come with high price tags. The balance between profit & patient welfare remains delicate.
Furthermore, healthcare reforms can shift economic landscapes. Policies impact affordability & accessibility of services. Recent changes highlight strains felt across The sector. Understanding these issues improves patient-provider interactions. As a participant in this arena, I’ve witnessed firsthand complexities faced daily. Managing costs remains a pressing concern for everyone involved.
Key Issues in Healthcare Economics
Many key issues exist within this field. One crucial aspect involves rising healthcare costs. These costs affect everyone in America. Patients often face escalating bills, causing financial strain. Providers must navigate reimbursement systems carefully. Inadequate reimbursements can lead To struggles maintaining quality care.
Another pressing issue surrounds access To healthcare. While many citizens possess insurance, coverage may not equal access. High co-pays deter patients from seeking help. Public health programs aim To address disparities. However, gaps remain, leading To avoidable complications. For additional information on healthcare costs, visit Americans’ Challenges with Health Care Costs.
Interrelationships within healthcare create further complexities. For example, provider-patient relationships shift under economic pressures. Patients may delay treatments due To costs. Providers worry about patient outcomes linked closely To economic factors. Research indicates significant flaws within U.S. healthcare finance models. More details can be found at A Dozen Facts About Healthcare Economics.
Patients’ Perspectives on Economics
Patients experience economic challenges firsthand. Rising premiums make budgeting challenging. Many Americans report difficulty affording care. Consequently, this drives them into debt. Mental health impacts emerge alongside financial pressures. Worry about healthcare expenses can lead To anxiety. This stress affects overall well-being, creating a cycle of hardship.
Healthcare costs can lead patients To avoid necessary treatments. They may delay seeking help for conditions. Postponing care often results in worsened health outcomes. Patients bear a heavy burden when weighing decisions. Increased costs tempt them To forego preventive services. This avoidance creates long-term complications for overall health.
Additionally, patients perceive unfairness under current economic structures. Unequal access results from various factors. Geographic location & socioeconomic status often determine care availability. Consequently, certain populations face more significant barriers. Providers must advocate for equitable access among all patients. Individual experiences highlight significant disparities within healthcare.
Providers’ Challenges in Healthcare Economics
Providers also navigate numerous economic challenges. Reimbursement rates fluctuate frequently. Insurance companies set these rates, impacting providers’ revenues. Insufficient compensation can affect service quality offered. Providers must adapt business models continuously. Many embrace technology while facing financial constraints.
Furthermore, high operational costs put pressure on practices. Salaries, equipment, & administrative expenses require careful management. Revenue cycles can become cumbersome, affecting cash flow. Providers experience stress when trying To balance budgets. Financial sustainability remains crucial To maintain quality care.
Changes within healthcare policies create additional complexity. Providers must stay informed about legislative changes. New regulations can affect reimbursement & compliance efforts. This shifting landscape demands agility from healthcare organizations. Continuous education helps navigate economic fluctuations effectively.
Addressing Economic Inequities
Addressing healthcare economic inequities requires proactive approaches. Policymakers must create frameworks promoting fairness. Targeting vulnerable populations can yield significant results. Programs aimed at underserved communities expand access considerably. Reducing economic barriers fosters improved health outcomes for everyone.
Moreover, collaboration among stakeholders offers solutions. Encouraging partnerships within communities can bridge gaps. Public-private collaborations drive meaningful change. Engaging local organizations helps promote awareness. Together, they can develop programs benefiting disadvantaged groups. Increased support for mental health services remains vital, too.
In addition, education plays a crucial role. Raising awareness about healthcare costs empowers patients. Informing them about options helps in navigating uncertainties. Resources such as financial counseling enhance patient autonomy. When patients feel informed, they can make better choices.
Technological Advances & Their Economic Impact
Technology plays a significant role in reshaping healthcare economics. Digital solutions streamline processes for providers. Telemedicine reduces costs associated with in-person visits. Patients benefit from increased accessibility & convenience. Technology adoption enhances patient satisfaction & outcomes.
Despite advantages, technology introduces new challenges. Initial investments can be prohibitive for many providers. Budget restrictions affect their ability To innovate. However, strategic planning can mitigate costs effectively. Providers must balance innovation with financial realities when investing.
Emerging technologies also change patient interactions. Online portals provide transparency regarding costs. Patients can access their medical records easily. Empowering them enhances their responsibility in healthcare decisions. This shift towards patient-centered care creates opportunities for improved outcomes.
Future Trends in Healthcare Economics
Emerging trends are shaping future healthcare economics. Value-based care models are gaining traction. Providers receive compensation based on patient outcomes. This approach incentivizes high-quality care delivery. Patients benefit from better health management while reducing costs.
Additionally, other innovations such as personalized medicine influence economics. Tailoring treatments To individuals leads To better results. However, this may also increase expenses. Understanding these dynamics is essential for all stakeholders. Trends indicate ongoing shifts in how healthcare finances operate.
Further advancements in artificial intelligence bring opportunities. AI aids in predicting patient needs & optimizing resources. These efficiencies can translate into significant savings. Providers can allocate resources more effectively. This potential transformation creates excitement regarding future possibilities.
Comparison of Economic Models
| Aspect | Fee-for-Service 🧾 | Value-Based Care 💡 | Capitation 💰 |
|---|---|---|---|
| Payment Structure | Per service provided | Based on patient outcomes | Fixed payment per patient |
| Focus | Volume of services | Quality of care | Prevention & efficiency |
| Risk | Provider risk increases | Shared risk | Provider bears risk |
| Patient Engagement | Limited engagement | Encourages active participation | Promotes preventive care |
Policy Changes Affecting Healthcare Economics
Policies shape healthcare economics significantly. Recent reforms aimed To improve accessibility. Changes promote affordable care for underserved communities. Providers must navigate new rules evolving constantly. Keeping up with regulations remains critical for operational success.
Healthcare reform discussions highlight various themes. Proposals focus on reducing costs, expanding access. Policymakers aim for affordable policies benefiting all parties. Building coalitions can strengthen advocacy for necessary changes. Engaging diverse stakeholders amplifies voices for reform.
Additionally, transparent communication about policies helps. Providers should keep patients informed about updates. Creating an environment of trust enhances patient-provider relationships. Collaborative approaches yield better health outcomes across systems.
Conclusion: A Complex & Evolving Landscape
Healthcare economics remains a complex & evolving landscape. Multiple factors influence interactions among providers & patients. Understanding these dynamics ensures better experiences for all. Continuous adaptation will be necessary in this field. Stakeholders must work collaboratively, seeking equitable solutions. With collective effort, we can navigate future challenges together.
Conclusion
Navigating The world of healthcare economics can be tough for both providers & patients. Rising costs, insurance complexities, & access To care are just a few hurdles everyone faces. It’s essential for patients To stay informed & ask questions while seeking help from providers who genuinely care. On The other hand, healthcare professionals need To balance their duties with The financial realities of running a practice. By working together & understanding each other’s challenges, both sides can find solutions that enhance care while managing costs more effectively. In The end, everyone deserves quality healthcare.