Navigating Quality of Care Challenges in Contemporary Healthcare Systems. Discover how To tackle quality care challenges in today’s healthcare systems. Explore practical tips & insights for better health outcomes & patient satisfaction.
What is Navigating Quality of Care Challenges in Contemporary Healthcare Systems & how does it work?
Navigating quality challenges means addressing healthcare delivery flaws. Systems need effective methods for improvement. Patients deserve high standards for safety. Providers must meet varied needs. Patient-centered care enhances overall experience.
Brief history of Navigating Quality of Care Challenges in Contemporary Healthcare Systems
Quality care has evolved over decades. Initially, focus remained on basic services. Increased complexity led To new challenges. Regulations were put in place as standards grew. Continuous feedback became essential for better practices.
How To implement Navigating Quality of Care Challenges in Contemporary Healthcare Systems effectively
Effective implementation requires clear strategies. Begin with assessing current operations. Engage staff in identifying gaps. Develop training programs for all levels. Use data analytics for informed decision-making.
Key benefits of using Navigating Quality of Care Challenges in Contemporary Healthcare Systems
Numerous advantages arise from quality navigation. Improved patient outcomes result from better care. Enhanced staff satisfaction leads To reduced turnover. Cost-efficiency improves with streamlined operations. Strong reputations build community trust.
Challenges with Navigating Quality of Care Challenges in Contemporary Healthcare Systems & potential solutions
Numerous obstacles exist when navigating quality challenges. Resistance among staff often hinders progress. Lack of funding can limit initiatives. Solutions include fostering open communication. Funding partnerships could support necessary changes.
Future of Navigating Quality of Care Challenges in Contemporary Healthcare Systems
Future trends showcase increasing technology use. Artificial intelligence may guide decision-making processes. Telehealth will become more mainstream, enhancing access. Data-driven approaches will refine practice standards. Quality assurance will remain a top priority.
Table of Navigating Quality of Care Challenges in Contemporary Healthcare Systems
| Challenge | Potential Solution |
|---|---|
| Staff resistance | Foster open communication |
| Lack of funding | Seek partnerships |
| Data overload | Utilize analytics tools |
| Patient engagement | Implement feedback systems |

Navigating Quality of Care Challenges in Contemporary Healthcare Systems
Quality of care remains vital across healthcare settings. Addressing quality concerns involves multiple stakeholders. Patients require effective interventions, while providers must ensure optimal service delivery. These aspects engage different facets in healthcare’s dynamic landscape. A recent experience reinforced this importance. During a family member’s recovery, navigating care accessibility proved challenging. Ensuring consistent communication among providers became essential. This scenario exemplifies interactions within healthcare systems.
Identifying Quality of Care Challenges
Recognizing challenges around quality of care serves as a critical first step. Many healthcare systems face complex issues affecting service delivery. Common challenges arise from fragmentation among various providers. Patients often encounter difficulties accessing necessary services. Lack of coordinated care may lead To inconsistent treatment experiences. Understanding specific needs helps in tailoring care solutions effectively. Emphasizing collaboration across healthcare disciplines can alleviate many identified challenges.
Quality metrics play a central role in this endeavor. Key indicators monitor patient outcomes & satisfaction. Analyzing these metrics informs improvements throughout healthcare facilities. Regular assessments ensure meaningful changes occur. Organizations like CMS (Centers for Medicare & Medicaid Services) provide resources for evaluating care quality. For more detailed information, visit Quality of Care.
Patient-centered care remains a fundamental goal. Using patient feedback enhances service delivery significantly. Providers should prioritize understanding patient experiences. Disparities identified within different populations require attention. Tailoring strategies towards diverse community needs fosters improved health outcomes. Moreover, addressing social determinants of health can positively impact service quality.
Strategies for Improvement
Implementing effective strategies proves essential for enhancing quality. Focused training programs ensure staff develop necessary skills. Continuous education empowers providers, enhancing their ability. Incorporating evidence-based practices into daily operations fosters improvement. Additionally, encouraging interdisciplinary collaboration plays a pivotal role. Teams that communicate effectively reduce errors & improve patient outcomes.
Technology also serves as a valuable resource. Electronic health records (EHR) support efficient information sharing. Streamlined access To patient data provides insight into treatment histories. Telehealth options have expanded access, especially in remote areas. Investing in modern health technologies increases healthcare quality noticeably. Learn more about quality assurance through resources provided by World Health Organization.
Utilizing data analytics enhances decision-making capabilities. Systems can analyze patient results against established benchmarks. Identifying trends supports quick adjustments in care delivery. Furthermore, establishing quality improvement committees encourages accountability among staff. Such groups monitor initiatives over time, ensuring quality strives remain ongoing. Creating a culture focused on continuous improvement plays a vital role.
Patient Engagement & Empowerment
Empowering patients extends beyond providing information. Patients should actively participate in their care decisions. Engaging individuals in treatment planning enhances trust & accountability. Educated patients often experience better health outcomes. Communication between providers & patients creates an environment conducive To care. Encouraging questions & discussions promotes healthy relationships.
Patient navigation services feature prominently in enhancing engagement. Navigators assist individuals in understanding available resources. They provide support throughout treatment processes, easing transitions. Moreover, feedback mechanisms allow patients To voice opinions on services received. Such insights empower providers, informing necessary adjustments. Ultimately, prioritizing patient voices shapes care experiences positively.
Healthcare systems must evolve alongside patient expectations. Modern individuals demand transparency & access To information. Organizations must adapt practices, fostering an open exchange. Emphasizing health literacy enhances patient understanding. Patients equipped with knowledge navigate systems more effectively. The shift towards patient-centered care represents a monumental change in healthcare philosophy.
Addressing Disparities in Healthcare Quality
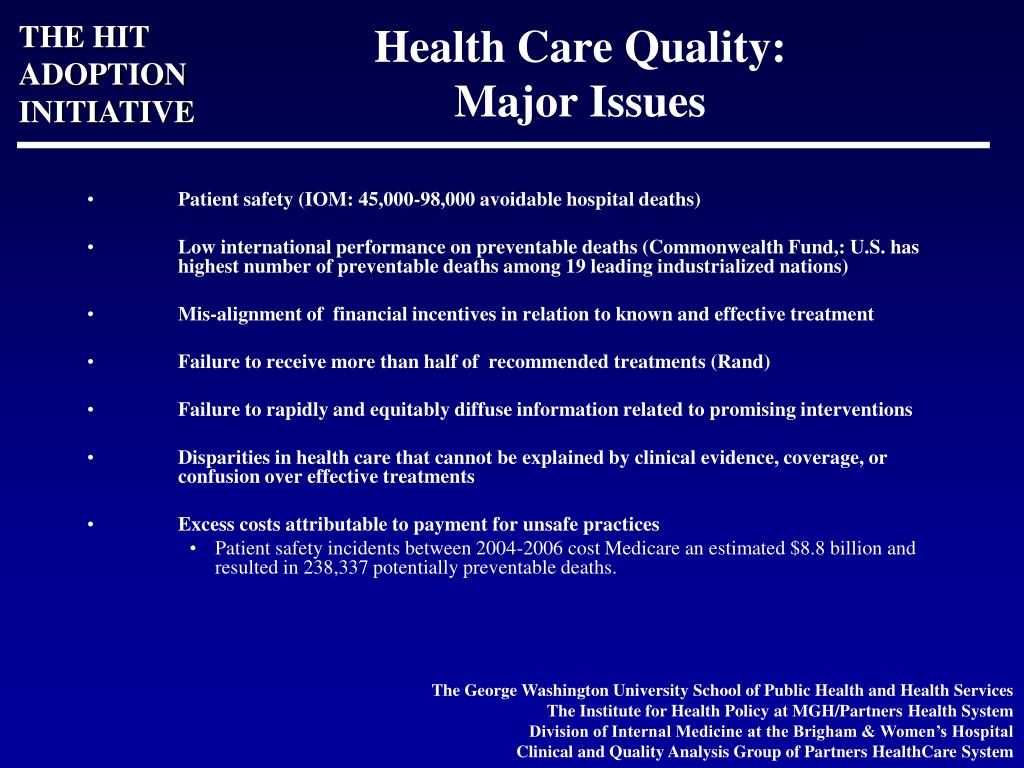
Healthcare disparities continue posing significant challenges. Many populations encounter barriers accessing quality services. Factors include socioeconomic status, geography, & race. Identifying these disparities highlights areas needing improvement. Communities facing higher risks require tailored interventions. Collaborative, community-based approaches prioritize health equity, ensuring everyone receives adequate care.
Public health initiatives can significantly impact marginalized areas. Outreach programs & educational campaigns increase awareness. Enhancing access To resources fosters healthier communities overall. Partnerships between healthcare systems & local organizations strengthen outreach efforts. Addressing systemic issues becomes integral in closing gaps in service delivery. Ultimately, changing systemic inequities drives significant innovations in care.
School & workplace health programs can serve as excellent resources. Encouraging healthy behaviors at early ages fosters long-term wellness. Everybody has a role in enhancing health equity across populations. Schools provide unique opportunities for health education. Workplaces can implement wellness programs benefiting entire communities.
Technological Advancements in Quality of Care
Technology impacts healthcare quality in profound ways. Innovations transform patient experiences significantly. For instance, AI-driven tools improve diagnostic accuracy. Advanced algorithms analyze data faster than human counterparts. These advancements support clinicians in making informed decisions. Moreover, automation reduces administrative burdens on healthcare providers. Streamlined processes allow staff To focus on direct patient care.
Telemedicine gained prominence recently, expanding access dramatically. Virtual consultations enable specialists To reach patients anywhere. This development particularly aids those in rural settings. Not only does telehealth enhance accessibility, but it also maintains quality. Regular follow-ups via virtual means can lead To better outcomes. Integrating telemedicine into standard practice represents a monumental shift.
Wearable devices offer another layer of health monitoring. Tracking vital signs provides real-time feedback on patient conditions. Such proactive measures can prevent severe health incidents. Data collected from wearables informs healthcare decisions directly. As technology continues evolving, quality of care improves alongside advancements.
Developing a Culture of Quality Improvement
Establishing a culture of quality improvement encourages staff engagement. Involving employees in decision-making fosters ownership over outcomes. Organizations benefit tremendously when employees feel valued & heard. Continuous feedback loops promote transparency & accountability. Encouraging staff participation enhances overall morale & reduces burnout, benefiting The entire system.
Quality tools & resources must become available throughout organizations. Access ensures teams can measure their performance effectively. Regular training sessions keep staff up-To-date with best practices. Moreover, celebrating successes reinforces positive behaviors & practices. Acknowledging achievements motivates continued efforts towards excellence.
Benchmarking against best practices allows organizations To identify weaknesses. Engaging in peer comparisons highlights areas needing development. Continuous learning must remain a core value for any healthcare organization. Participating in external audits reveals insights that drive quality enhancements. Ultimately, building a robust culture around quality reinforces systemic improvements.
Future Directions for Quality of Care
Looking ahead, navigating quality of care challenges demands resiliency. Healthcare systems must adapt continually To evolving needs. Shifting demographics & technological advancements impact strategies directly. Fostering interdisciplinary approaches encourages shared responsibility among providers. Collaboration leads To holistic care experiences, enhancing overall service quality.
As patient expectations evolve, so must delivery methods. Emphasizing prevention over treatment reshapes healthcare frameworks. Prioritizing holistic approaches focuses on an individual’s well-being. Integrated care models consider various aspects of health while delivering services. Strong partnerships extend beyond traditional roles, building comprehensive support systems.
Future research must focus on innovative solutions that reshape care delivery. Understanding patient perspectives fosters greater collaboration. Embracing emerging technologies ensures healthcare remains forward-thinking. Ultimately, navigating quality of care challenges relies on collective effort. Stakeholders across various sectors must unite for meaningful change.
Key Features in Navigating Quality of Care
- Patient-centered care models 🤝
- Interdisciplinary collaboration 🤝
- Continuous staff training 📚
- Data-driven decision-making 📊
- Community engagement initiatives 🌍
- Technology integration in health 🚀
- Monitoring & evaluation systems 📈
What is quality of care in healthcare?
Quality of care refers To The degree To which healthcare services for individuals & populations increase The likelihood of desired health outcomes. It is based on The best available evidence & is intended To provide care that is safe, effective, patient-centered, timely, efficient, & equitable.
How is quality of care measured?
Quality of care can be measured through various indicators, including patient outcomes, patient satisfaction surveys, adherence To clinical guidelines, & The rates of medical errors or complications. Various organizations also use benchmarks & data analytics To monitor & assess quality performance.
What role do healthcare professionals play in ensuring quality of care?
Healthcare professionals, including doctors, nurses, & allied health staff, play a crucial role in ensuring quality of care by adhering To best practices, engaging in continuous education, fostering communication with patients, & participating in quality improvement initiatives within their organizations.
Why is patient safety important in quality of care?
Patient safety is a fundamental component of quality care as it aims To prevent harm To patients during The provision of healthcare services. Ensuring patient safety leads To better health outcomes, increased patient trust, & reduced healthcare costs associated with avoidable adverse events.
What impact does patient satisfaction have on quality of care?
Patient satisfaction is an important indicator of quality of care as it reflects patients’ experiences & perceptions of The services they receive. High levels of satisfaction are often associated with better adherence To treatment plans, improved health outcomes, & increased likelihood of patients returning for future care.
How can healthcare organizations improve The quality of care?
Healthcare organizations can improve The quality of care by implementing evidence-based practices, conducting regular training & education for staff, utilizing data analytics To monitor performance, engaging patients in their care, & fostering a culture of safety & continuous improvement.
What are common quality of care issues faced in healthcare?
Common quality of care issues include medication errors, inadequate staffing, poor communication among healthcare providers, failure To follow clinical guidelines, patient falls, & hospital-acquired infections. Addressing these issues is vital for improving overall care quality.
How does technology influence quality of care?
Technology influences quality of care by enabling better data management, facilitating communication among healthcare providers, & enhancing patient engagement through telemedicine & health apps. Electronic health records improve The accessibility of patient information, which can lead To improved clinical outcomes.
What is The significance of evidence-based practice in quality of care?
Evidence-based practice is significant for quality of care as it integrates The best available research evidence with clinical expertise & patient values. This approach ensures that healthcare practices are based on The latest scientific findings, leading To more effective & safer care for patients.
How does access To care affect quality of care?
Access To care significantly affects quality of care as it determines whether individuals are able To obtain necessary preventive, curative, & rehabilitative services. Barriers To access, such as cost, transportation issues, & provider availability, can lead To delayed care, worsened health outcomes, & disparities in treatment.
What role does accreditation play in quality of care?
Accreditation plays a critical role in ensuring quality of care by establishing standards for healthcare organizations & providing a framework for evaluation. Accreditation bodies assess compliance with these standards, helping To ensure that facilities are delivering safe & effective care To patients.
Navigating Quality of Care Challenges in Contemporary Healthcare Systems
Understanding Quality of Care
Quality of care represents a multi-faceted concept. Many healthcare providers focus on a patient-centered approach. To enhance patient experience, systems need ongoing evaluation. Clinicians should continually assess outcomes & patient feedback. These elements help in improving overall service delivery. Effective communication remains vital among caregivers. Patients must feel valued & understood during interactions. Furthermore, education plays a crucial role in ensuring high-quality care.
Healthcare organizations need robust frameworks for quality measurement. Regulatory guidelines help outline expectations for performance. Utilizing standardized metrics enables effective comparison across different settings. These metrics can range from patient satisfaction scores To clinical outcome indicators. By adopting comprehensive quality frameworks, systems can identify gaps. A proactive approach fosters improvement & encourages transparency.
Investing in staff training enhances quality delivery. Empowering healthcare professionals results in better patient outcomes. Motivated staff tend To prioritize care & demonstrate compassion. In this dynamic healthcare environment, an adaptable workforce exhibits resilience. Yet, organizations must navigate workforce challenges amidst changing demands. Ongoing training ensures that personnel remain updated on best practices.
Challenges in Ensuring Quality Care
Multiple factors contribute To challenges within healthcare delivery systems. Limited resources can lead To compromised care quality. Insufficient staffing levels place undue pressure on available personnel. Stress often diminishes attentiveness, resulting in errors. Furthermore, healthcare facilities sometimes struggle with outdated technologies. Upgrading infrastructure requires significant financial investment, often hampering progress.
Accessing quality care remains a persistent obstacle. Many patients experience barriers like cost & location. Disparities exist among marginalized communities, hindering equitable access. Effective solutions require collaboration among stakeholders. Policymakers should prioritize initiatives aimed at closing care gaps. Addressing these issues ensures that all individuals receive quality service without obstruction.
Additionally, regulatory burdens can impact quality. Meeting multiple compliance requirements consumes valuable resources. Healthcare organizations must balance compliance with provisions for patient care. This balancing act can lead To inefficiencies. Managing these complexities often detracts from direct patient interaction. Flexibility in regulations may promote better outcomes for patients in diverse settings. More information about healthcare systems can be found at this resource.
Patient Engagement in Quality Improvement
Patient engagement efforts contribute significantly To quality improvements. Informed patients can make better healthcare decisions. Involving them in care decisions strengthens provider-patient relationships. They should have access To relevant information regarding their health. Accessibility To educational resources empowers patients & promotes autonomy. Tools for self-management further enhance their engagement levels.
Healthcare providers must prioritize communication with patients. Effective dialogue fosters transparency & trust. Regular feedback mechanisms should be implemented. This allows patients To voice concerns & suggestions. Organizations can use these insights for implementing meaningful improvements. Systems that embrace patient feedback tend To show better outcomes. Detailed strategies for enhancing this engagement may be found on this site.
Furthermore, tailored care plans enhance patient satisfaction. Customization based on individual preferences leads To improved experiences. Patients feel more valued when they have a say in their care. As a result, they are more likely To comply with treatment protocols. Empowering patients not only fosters trust but ultimately enhances care quality. A personal experience reminded me of this power. By openly discussing treatment options with my doctor, I felt more engaged.
Role of Technology in Quality Care
Technology plays a vital role in modern healthcare systems. Implementing electronic health records (EHR) enhances information accessibility. EHR systems allow for effective data sharing across providers. This results in better coordination & informed care decisions. Patient histories become easily retrievable, minimizing chances for errors. Technology streamlines processes, increasing efficiency among healthcare staff.
Telemedicine expands access, especially in underserved areas. Patients can consult with healthcare providers remotely. This flexibility eliminates geographical barriers To receiving care. In addition, monitoring tools allow patients To manage chronic conditions effectively. Wearable devices track vital signs, alerting providers if issues arise. Overall, technology acts as a crucial facilitator of quality care.
However, challenges accompany technology integration. Training staff To use new tools can be resource-intensive. There may exist resistance among some personnel. Overcoming this barrier requires a culture shift within organizations. Emphasizing ongoing learning & adaptability enhances staff buy-in. As systems evolve, technology must align with quality goals, maximizing patient benefit.
Measuring Quality Care Outcomes
Measuring quality care outcomes remains critical in evaluating effectiveness. Various metrics provide insights into care delivery. Traditionally, clinical outcomes like morbidity & mortality rates served as key indicators. Patient-reported experiences now add another dimension of assessment. Organizations must analyze these metrics continuously for improvement. Reviewing performance data can reveal trends & potential issues.
Benchmarking against best practices helps identify strengths & weaknesses. Organizations should collaborate To share successful methodologies. Learning from peers promotes collective growth within healthcare systems. Engaging in quality improvement collaboratives can bridge gaps. Organizations with similar challenges may find solutions by working together. Regular assessments aid in sustaining a high standard of care.
Furthermore, adopting advanced data analytics yields deeper insights. Predictive modeling can identify at-risk patients early. Proactive approaches drive interventions before challenges escalate. Consistently measuring outcomes informs strategic planning. Continuous quality enhancement remains a shared responsibility among all stakeholders. By adopting metrics-based evaluations, systems ensure accountability for care quality.
Comparative Analysis of Quality of Care Challenges
| Factor | Traditional Systems | Modern Systems | Patient Engagement | Technology Integration |
|---|---|---|---|---|
| Access To Care | Limited resources 😟 | Greater reach 🌐 | High barriers 🚧 | Global access 🔗 |
| Staff Training | Rudimentary training 🏫 | Ongoing development 📚 | Patient education 🙋♂️ | Tech training 💻 |
| Quality Metrics | Static evaluations 📊 | Dynamic assessments 📈 | Feedback-driven 🔄 | Data analysis 🔍 |
Strategies for Navigating Quality Care Challenges
Proactive strategies promote resilience within healthcare systems. Organizations should focus on continuous quality improvement. Implementing evidence-based practices enhances care delivery. Regularly assessing performance metrics allows for timely adjustments. This cyclical approach fosters a culture of excellence. Systems must prioritize communication across departments To share insights.
Collaboration among stakeholders drives successful innovation. Engaging community organizations creates awareness of available resources. Supporting patients holistically enhances their experience within healthcare. Emphasizing shared goals encourages multidisciplinary teamwork. Addressing workforce challenges requires unity within organizations. A strong, supportive environment fosters motivation among healthcare professionals.
Finally, leveraging technology supports quality improvement initiatives. Investing in advanced systems enables efficient data management. Ensuring accessibility of information empowers both patients & providers. By streamlining workflow processes, organizations enhance efficiency. All these measures contribute To building resilient, quality-focused healthcare systems. Persistent collaboration remains essential for overcoming ongoing challenges within The landscape.
Conclusion
In today’s healthcare world, tackling quality of care challenges is essential for better patient experiences. Everyone involved—patients, providers, & policymakers—needs To work together. Simple steps, like improving communication & using technology wisely, can make a big difference. By focusing on what truly matters, we can ensure that everyone gets The care they deserve. Let’s keep striving for a system where high-quality care is The norm, not The exception. Together, we can create a healthier future for all, filled with compassion & support. Embracing these changes is key for improving lives in our communities.
