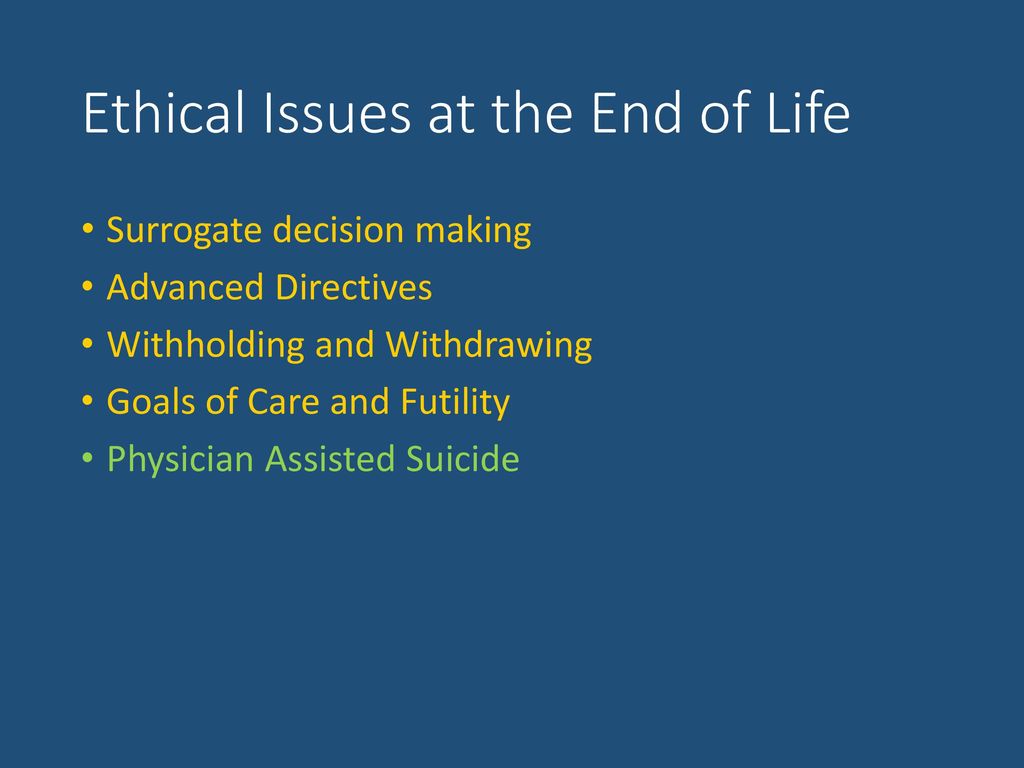
Ethical Dilemmas in End-of-Life Care: Balancing Compassion and Patient Autonomy. Explore how To handle tough choices in end-of-life care, focusing on compassion & respecting patient wishes. Discover a balanced approach To these ethical questions.
What is Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy & how does it work?
Navigating ethical dilemmas involves making tough choices. Compassion & patient autonomy play crucial roles. Compassion focuses on empathy & support. Patient autonomy emphasizes individual rights & wishes. Many healthcare professionals face conflicts in these areas. Finding balance ensures respectful decision-making processes.
Brief history of Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy
This concept has evolved over many years Ethical Dilemmas in End-of-Life Care. Early practices often overlooked patient wishes. Focus shifted from paternalism towards empowering patients. Awareness of ethical considerations has grown significantly. Regulatory frameworks have also developed alongside these changes. Society now values informed consent & open dialogue.
How To implement Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy effectively
Effective implementation requires training staff regularly. Open communication with patients fosters trust & understanding. Incorporating interdisciplinary teams enhances diverse perspectives. Establishing clear protocols aids decision-making processes. Ensuring policies align with ethical standards promotes better care. Continuous evaluation of practices leads To improvements.
Key benefits of using Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy
Several benefits arise from balanced approaches. Increased patient satisfaction occurs when wishes are honored. Stronger relationships form between patients & caregivers. Ethical decision-making fosters respect for human dignity. Healthcare teams experience reduced conflict & stress. Improved outcomes result from holistic consideration of needs.
Challenges with Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy & potential solutions
Several challenges can emerge during this process. Conflicting values among team members often arise. Cultural differences impact patient perspectives significantly. Communication barriers may hinder effective dialogue. Solutions exist, including ongoing education & training. Establishing clear, respectful channels for discussions improves outcomes.
Future of Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy
Future trends suggest ongoing evolution in this area. Technology will enhance communication & data sharing. Telemedicine may increase access To specialized care. Growing emphasis on shared decision-making will shape practices. Continued research will refine ethical guidelines & frameworks.
Table of Navigating Ethical Dilemmas in End-of-Life Care: Balancing Compassion & Patient Autonomy
| Aspect | Importance | Strategies |
|---|---|---|
| Compassion | Enhances patient experience | Training programs |
| Patient Autonomy | Supports individual rights | Clear consent forms |
| Team Collaboration | Improves decision-making | Interdisciplinary meetings |
| Communication | Builds trust | Open dialogue sessions |
| Cultural Sensitivity | Respects diverse backgrounds | Training on cultural competence |
Navigating Ethical Dilemmas in End-of-Life Care
In healthcare, professionals often face tough choices. Ethical dilemmas arise, especially in end-of-life scenarios. Balancing compassion with patient autonomy remains crucial. These challenges demand sensitivity, understanding, & respect for patients’ rights.
Understanding Patient Autonomy
Patient autonomy refers To individuals’ rights To make decisions about their care. This principle empowers patients. Many believe they should have control over their healthcare choices, especially during end-of-life care. Ensuring understanding of one’s health status influences decision-making significantly.
Every healthcare provider must respect patient autonomy. Some guidelines emphasize informed consent. Patients should receive all information about their conditions. Knowledge helps them make educated choices. This process becomes especially critical when advanced care planning occurs, as individuals express desires for future treatment. You can learn more from this article.
Healthcare professionals may encounter situations where patient autonomy conflicts with their beliefs. Providers may struggle when patients refuse treatment. In such cases, discussions become necessary. Providers must facilitate conversations while respecting individual choices. Empathy plays an important role in fostering trust throughout this process.
The Role of Compassion in Care
Compassion becomes vital during end-of-life decisions. Healthcare workers should support patients with empathy & kindness. Listening attentively ensures patients feel valued. Compassionate care helps ease anxiety in difficult times. Patients often appreciate providers who go beyond clinical duties.
Providers should find ways To communicate effectively. Discussing fears, hopes, & preferences require patience. Compassion enables providers To guide patients through complex decision-making processes. This connection enhances understanding & promotes a supportive environment.
Sometimes, compassionate care might seem in conflict with patient autonomy. Providers may feel torn when patients request aggressive treatments. Balancing these concepts becomes challenging. Compassionate care aims for patient comfort while respecting their wishes. Acceptance of diverse perspectives in end-of-life decisions remains key, as fostering informed discussions aids in achieving this balance.
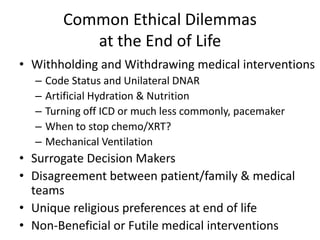
Ethical Principles at Play
Several ethical principles guide end-of-life care. Beneficence requires providers To act in patients’ best interests. Non-maleficence emphasizes avoiding harm. These principles guide decisions regarding treatments or interventions. Balancing these ethical tenets creates a framework for navigating dilemmas.
Justice plays a role, ensuring fair distribution of healthcare resources. In many cases, patients receive recommendations based on clinical guidelines. However, these guidelines may not always align with individual circumstances. Hence, providers must balance adherence To established standards & respect individual patient preferences.
When discussing ethical dilemmas, integrity comes into play. Providers must remain steadfast in adhering To ethical standards while managing conflicting interests. For instance, conflicts between personal beliefs & professional obligations often arise. When facing such moments, clear communication may help bridge differences & enhance collaboration.
When Patient Wishes Conflict with Family Opinions
Family input often influences patients’ healthcare decisions. Disagreements might arise when patients express preferences contrary To family desires. These conflicts can lead To emotional tension & heightened distress for all parties involved. Sometimes, family members struggle with accepting patients’ choices for various emotional reasons.
Healthcare providers must manage these disputes delicately. Open communication fosters dialogue among all involved. By inviting family members into discussions, providers can clarify patients’ perspectives. Listening To family concerns while reiterating patient autonomy allows for a balanced approach.
Support groups may aid in mediating family disagreements. Involving ethics consultants can provide additional layers of support. When all stakeholders understand concerns, finding common ground becomes easier. This collaboration nurtures an environment conducive To heartfelt conversations.
Legal Considerations in End-of-Life Care
Legal aspects add complexity To end-of-life decision-making. Advance directives & living wills enable patients To express wishes beforehand. Understanding these documents helps ensure legality & adherence To patient’s desires. Providers must familiarize themselves with state laws surrounding end-of-life care.
Healthcare professionals may face legal repercussions for disregarding advance directives. Ensuring documentation reflects accurate patient intent saves future conflicts. Conversations regarding these documents often empower patients & solidify their autonomy. Encouraging timely discussions around advance care planning remains essential.
In cases where legal guardians are involved, complicating factors may arise. Providers must navigate relationships carefully. Keeping lines of communication open between patients, families, & clinicians helps mitigate potential conflicts. Each party deserves consideration, leading toward clearer understanding of healthcare choices.
Shared Decision-Making in End-of-Life Care
Shared decision-making empowers patients by involving them in care choices. Providers should facilitate relationships that prioritize collaboration. Engaging in discussions & exploring treatment options together promotes transparency. Sharing test results & prognosis creates informed environments.
Providers can utilize decision aids that present treatment options clearly. Such tools enhance understanding & improve patient engagement. Visual representation helps demystify complex medical concepts & invites meaningful dialogue. This practice fosters relationships grounded in trust & respect.
Ultimately, shared decision-making transcends mere communication. Developing a mutual understanding nurtures relationships & supports compassion. Creating spaces where patients express their values ensures personalized care. Providers championing shared decision-making honor patient dignity while navigating ethical considerations.
The Impact of Cultural Perspectives
Cultural backgrounds greatly influence end-of-life decision-making. Each culture carries unique beliefs about death & dying. These perspectives shape patients’ values & attitudes towards medical interventions. Awareness of individual cultural contexts bolsters advocates for compassionate care.
Providers integrated within cultural spheres nurture relationships built on trust. Culturally competent care pays respect To traditions & beliefs. As providers learn more about patients’ backgrounds, care becomes more personalized & mindful. This insight fosters beneficial conversations about end-of-life preferences.
Healthcare settings should address cultural needs effectively. Offering multilingual resources or culturally-sensitive staff members exemplifies commitment. Recognizing diverse perspectives enhances responsiveness & patient autonomy. Inclusion fosters environments where patients feel safe expressing beliefs & values.
Examples of Ethical Dilemmas in End-of-Life Care
Many real-life scenarios highlight ethical dilemmas in end-of-life care. A patient with terminal cancer may wish for aggressive treatment. Family members may hope for a peaceful transition without interventions. This disagreement showcases conflicts between individual desires & familial expectations.
Another example involves unrestricted use of life support. Some families advocate for prolonging life at all costs. Conversely, The patient may have expressed a wish against such measures. Balancing these conflicting wishes necessitates thoughtful conversations among all parties.
Finally, consider instances where organ donation arises. Patients may wish To donate organs, while families may struggle with this decision. Concerns regarding loss of autonomy or premature death often surface. Sensitivity & support are essential in navigating such deeply personal issues.
Promoting Advance Care Planning
Advance care planning emphasizes proactive discussions surrounding end-of-life preferences. Encouraging these dialogues prepares patients, families, & providers alike. Healthcare systems should integrate advanced care planning into routine care. This integration minimizes later conflicts & enhances patient satisfaction.
Many resources exist supporting advance care planning initiatives. Documents such as advance directives & POLST forms facilitate communication. These instruments spell out individuals’ wishes, bridging gaps between decisions & intentions. Educating patients about their options fosters greater understanding & involvement.
Providers can initiate advance care planning conversations during routine visits. Fostering a casual environment encourages open dialogue surrounding preferences. Educated patients are more likely To express wishes confidently, alleviating burdens upon families & improving quality of care.
Continuing Education for Healthcare Professionals
Ensuring healthcare professionals possess current knowledge remains vital. Continuous education equips them with tools for navigating ethical dilemmas. Workshops & seminars provide necessary updates on evolving ethical frameworks & best practices. This knowledge empowers providers To act compassionately in challenging scenarios.
Furthermore, collaboration among healthcare professionals fosters a shared understanding of ethical considerations. Teaming up with ethicists can enhance capability in handling complex situations. Professionals must keep abreast of legal changes surrounding end-of-life care, ensuring adherence To guidelines.
Participation in interdisciplinary meetings promotes holistic approaches To ethical dilemmas. Sharing experiences enables providers To learn from one another. Packed with diverse perspectives, collaboration strengthens healthcare systems in addressing patients’ end-of-life needs.
Navigating Emotional Turmoil
Healthcare professionals may experience emotional struggles while navigating ethical dilemmas. Witnessing patients’ suffering can be challenging Ethical Dilemmas in End-of-Life Care, often evoking strong feelings of empathy. Personal emotional responses require monitoring among compassionate practitioners. Self-awareness & emotional intelligence enhance effectiveness in providing care.
Applying self-care strategies aids healthcare professionals in managing stress. Establishing boundaries & seeking support creates a healthier work environment. Collaborating with peers within support systems provides reassurance & nurtures resilience. Engaging in reflective practices enhances emotional processing skills.
Utilizing debriefing sessions following challenging cases can also benefit staff. These discussions create spaces for emotional expression, promoting healing & growth. Strengthening emotional well-being helps sustain compassion in future encounters while bolstering resilience in intensive environments.
Key Features of Navigating Ethical Dilemmas
- Empowering patient autonomy 🤲
- Facilitating compassionate care 💖
- Incorporating family perspectives 🏡
- Utilizing shared decision-making 🤝
- Embracing cultural differences 🌍
- Encouraging continuous professional development 📚
What are The main ethical principles involved in end-of-life care?
The main ethical principles in end-of-life care include autonomy, beneficence, non-maleficence, & justice. Autonomy relates To respecting The patient’s wishes & choices, beneficence emphasizes acting in The patient’s best interest, non-maleficence involves avoiding harm, & justice pertains To providing fair treatment & access To care.
How does patient autonomy influence end-of-life decisions?
Patient autonomy is a fundamental principle that grants individuals The right To make decisions about their own medical treatment, including end-of-life care. This principle supports The belief that patients should have The ability To refuse or choose specific treatments based on their values & beliefs, even if their decisions may not align with medical recommendations.
What role does informed consent play in end-of-life care?
Informed consent is crucial in end-of-life care as it ensures that patients understand their diagnosis, treatment options, & potential outcomes. Healthcare providers must communicate clearly & allow patients or their surrogates To make decisions that reflect their preferences, thus upholding The ethical principle of autonomy.
How can healthcare providers address conflicts with family members regarding end-of-life care?
Healthcare providers can address conflicts with family members by facilitating open & honest communication. They should encourage discussions that include The patient’s wishes, provide education on The patient’s condition & prognosis, & mediate To help align family perspectives with The patient’s autonomy & care goals.
What is The significance of advance directives in end-of-life care?
Advance directives hold significant importance as they allow patients To outline their preferences for medical treatment in advance, particularly when they may become unable To communicate their wishes. They promote autonomy & ensure that healthcare providers & family members understand The patient’s desires regarding end-of-life decisions.
How can cultural beliefs impact ethical decision-making in end-of-life care?
Cultural beliefs can profoundly influence ethical decision-making in end-of-life care, as different cultures may have distinct beliefs about death, dying, & The afterlife. Understanding these cultural perspectives is essential for healthcare providers To ensure that care approaches are respectful & aligned with The patient’s values & customs.
What challenges do healthcare providers face in ensuring equitable access To end-of-life care?
Healthcare providers often face challenges in ensuring equitable access To end-of-life care, including disparities in healthcare resources, socioeconomic factors Ethical Dilemmas in End-of-Life Care, & varying levels of health literacy among patients. It is essential for providers To advocate for policies that promote equitable care & address these disparities To ensure that all patients receive The support they need.
What is The ethical debate surrounding assisted dying or euthanasia?
The ethical debate surrounding assisted dying or euthanasia centers on The conflict between respecting patient autonomy & concerns about potential abuses or The sanctity of life. Supporters argue that individuals should have The right To choose a dignified death, while opponents worry about The implications for vulnerable populations & The role of healthcare providers.
How can healthcare teams support The emotional needs of patients & families at The end of life?
Healthcare teams can support The emotional needs of patients & families by providing compassionate care, facilitating open communication, & offering resources like counseling & support groups. Addressing psychological, spiritual, & social needs is as important as physical care, ensuring a holistic approach To end-of-life care.
What ethical considerations are involved in The use of palliative care?
Ethical considerations in palliative care include The principles of beneficence & non-maleficence, focusing on relieving suffering & improving quality of life without hastening death. Providers must balance aggressive symptom management with The potential for sedatives or opioids To influence The timing of death, always prioritizing The patient’s goals & wishes.
.jpg)
Navigating Ethical Dilemmas in End-of-Life Care
Understanding Patient Autonomy
Patient autonomy stands as a cornerstone of modern healthcare. Individuals desire control over decisions related To their health. In end-of-life scenarios, patients often face profound choices. Respecting autonomy means honoring informed consent. This principle empowers patients, allowing them decision-making power. Each person’s values & beliefs shape their healthcare preferences. Thus, discussions around treatment options emerge in these critical moments.
A deep understanding of patient perspectives enhances care. Clinicians must actively engage patients in meaningful conversations. This engagement fosters trust & collaboration in decision-making. Questions about quality of life often arise. Patients appreciate clarity regarding prognosis & treatment benefits. As providers, maintaining empathy during these discussions proves vital.
Legal aspects also intertwine with autonomy. Advanced directives guide healthcare providers during unresponsive periods. These documents outline a patient’s wishes regarding care. Issues occur when family members conflict about desired treatments. Respecting a patient’s wishes remains paramount, requiring thoughtful navigation by caregivers. Navigating these waters becomes essential in critical moments of decision-making.
Compassion in End-of-Life Care
Compassion represents a fundamental aspect in providing care at life’s end. Offering emotional support eases distress for both patients & families. Professional caregivers must recognize this pain while addressing medical needs. Empathy enables practitioners To connect deeply with patients. Recognizing emotional turmoil enhances overall care quality.
Surrogates often play significant roles in The decision-making process. Caregivers must provide reassurance, helping them understand patient wishes. In these situations, compassion bridges gaps between misunderstanding & support. Communication becomes crucial; it transforms fear into trust. The compassion exhibited during this journey leaves lasting impressions.
Cultural sensitivity enhances compassionate care. Different cultures perceive end-of-life experiences uniquely, impacting decisions. Understanding these nuances ensures that professionals honor diverse values. Compassionate interactions enhance patients’ sense of dignity. This respect creates an environment conducive To open discussions about care preferences.
Ethical Principles in End-of-Life Care
Four primary ethical principles guide end-of-life care: autonomy, beneficence, non-maleficence, & justice. Autonomy grants patients control over decisions. Beneficence emphasizes promoting good & well-being. Non-maleficence urges avoidance of harm in care decisions. Finally, justice requires equitable healthcare access for all individuals.
Balancing these principles can prove challenging for healthcare providers. For instance, a patient’s wish for aggressive treatment might conflict with The principles of beneficence & non-maleficence. Navigating these conflicting demands requires skill & sensitivity. Conversations focused on values foster understanding between parties, guiding ethical decision-making.
Additionally, ethical frameworks offer guidance. Frameworks encourage clinicians To reflect on moral dilemmas. These approaches often incorporate shared decision-making strategies. Such techniques cultivate empathy & trust among everyone involved. Navigating ethical landscapes in end-of-life care demands continual self-reflection.
Learn more about ethical frameworks in healthcare here.
Advanced Directives & Choices
Advanced directives allow individuals To specify their healthcare preferences. Patients express desires regarding treatment options through these documents. Discussing these directives early proves crucial in care planning. This proactive approach ensures patients’ wishes remain central throughout care processes. Advanced directives reduce conflicts within families during critical moments.
Healthcare professionals encourage discussions about these plans. Such conversations facilitate understanding among patients & their families Ethical Dilemmas in End-of-Life Care. Individuals often experience relief by expressing their choices openly. Providers should approach these discussions with sensitivity, ensuring patients feel heard. This creates pathways for better care that aligns with individual desires.
In some cases, healthcare teams face challenges honoring these directives. Issues arise when family members disagree with patient wishes. Providers must navigate these concerns diplomatically. Open communication among all parties remains essential for resolution. Respecting established advanced directives fosters trust throughout care experiences.
Explore best practices for respecting patients’ wishes here.
Communication Strategies
Effective communication proves essential in navigating ethical dilemmas. Open dialogues promote understanding among patients, families, & providers. Utilizing active listening encourages connection during challenging discussions. Practitioners must remain present, validating emotions expressed by patients. This practice enhances trust, allowing for smoother decision-making processes.
Using clear, straightforward language fosters comprehension. Avoiding medical jargon keeps families informed. Providing information helps patients feel empowered in their care journey. Discussing prognosis, treatment options, & possible outcomes creates shared understanding. Continuous engagement through open dialogue allows patients’ concerns To surface.
Establishing interdisciplinary teams enhances communication. Engaging various professionals ensures comprehensive, holistic care. Each member contributes perspectives shaped by unique experiences. Collaboration fosters an environment where complex decisions can surface. A unifying approach can lead To better outcomes, fulfilling ethical obligations while promoting compassion.
Experiences from Practice
In my experience as a healthcare provider, navigating end-of-life care brings challenges. Each encounter involves delicate discussions about patient wishes. Witnessing families struggle with conflict highlights essential communication barriers. I learned To listen actively & engage meaningfully during these moments. Each interaction has taught me invaluable lessons about compassion & respect.
Respecting patients’ desires in care fosters trust & a sense of dignity. I often face emotional complexities in these discussions. Compassionate responses create a supportive environment for families. Empathy plays a pivotal role in helping families make informed choices. Remembering each patient’s uniqueness leads us closer To personalized care.
My journey continues, & I strive for continuous learning. Engaging with diverse families broadens my understanding of cultural nuances. This experience has reinforced my commitment To providing compassionate care. Every moment spent with patients enriches my perspective on life & death. I remain dedicated To improving my practice & supporting others in these sensitive situations.
Balancing Compassion & Ethical Considerations
Creating balance between compassion & ethics fosters good healthcare practices. Professionals must engage with both principles throughout care processes. Ethical dilemmas often challenge providers, pushing them toward difficult choices. Maintaining compassion while navigating these challenging waters proves essential. Striking that balance can significantly impact patient & family experiences.
Organizations should support staff in managing these dilemmas. Offering training enhances clinicians’ skills in ethical decision-making. Encouraging networking among professionals fosters peer-To-peer learning. Sharing experiences equips providers with tools necessary for effective communication. Ongoing education empowers teams To navigate conflicts adeptly.
Ultimately, fostering compassionate care amid ethical dilemmas enhances healthcare delivery. All team members should prioritize open-mindedness & empathy. Understanding perspectives of those involved forms a strong foundation. By prioritizing compassion, providers can navigate challenges effectively. This approach leads To improved outcomes for patients & their families.
Comparative Table of Ethical Dilemmas
| Aspect 🤝 | Compassion 💖 | Patient Autonomy 🌟 |
|---|---|---|
| Decision-Making | Focus on emotional support | Emphasis on informed choices |
| Patient Engagement | Promotes open dialogue | Respects individual values |
| Team Collaboration | Encourages multidisciplinary approach | Supports families in decisions |
| Cultural Sensitivity | Honors diverse backgrounds | Incorporates unique beliefs |
| Outcome Focus | Enhances overall well-being | Empowers patient choices |
Future Directions in End-of-Life Care
Improvements in end-of-life care continue To evolve. New research explores innovative strategies for practice. Clinicians must focus on integrating technology into care frameworks. Telehealth options expand access for patients seeking consultations. These developments alleviate burdens associated with transportation. Incorporating digital tools remains crucial for enhanced dialogue.
Emerging ethical challenges necessitate ongoing education. Teams must stay abreast of changing laws & regulations. Continuous training improves competency in managing diverse situations. Ethical committees can provide additional support, guiding providers through dilemmas. This collaborative network strengthens care delivery & ethical practices.
Patient-centered care remains an essential objective Ethical Dilemmas in End-of-Life Care. Organizations should prioritize creating environment conducive To open conversations. Encouraging shared decision-making fosters trust. Individualized plans highlight unique patient needs & preferences. Ongoing efforts will promote compassion & autonomy in end-of-life care.
Conclusion
In end-of-life care, finding The right balance between compassion & respecting a patient’s choices can be tough. It’s important To listen & understand what The patient wants while also considering their loved ones. Ethical dilemmas often arise, but open conversations can help guide decisions. By focusing on empathy, clear communication, & teamwork, healthcare providers can support patients through this sensitive time. Ultimately, honoring a person’s wishes while showing kindness helps create a peaceful end-of-life experience. Together, we can navigate these challenges with heart & respect, ensuring that care aligns with individual values & needs.